Parkinson’s Disease (PD) affects nearly 100,000 Canadians and 10 million people worldwide. Characterized by a dopamine deficiency in the brain, this neurodegenerative disease disrupts signal transmission in the brain, impacting its proper functioning. Motor symptoms, like tremors, slowness of movement and imbalance problems can appear and deteriorate in patients who have quietly carried the disease for years. Equally devastating are PD’s lesser-known symptoms, like depression, anxiety, hallucinations, dizziness and sleep disorders.
While there is currently no cure for PD, a team of researchers at the Neuro (Montreal Neurological Institute-Hospital) has been advancing PD research through groundbreaking innovation. Led by Thomas Durcan, Associate Professor in the Department of Neurology and Neurosurgery at McGill and Director of the Neuro’s Early Drug Discovery Unit, the team has applied stem cell technology to create human organoids.
Organoids are minuscule, three-dimensional tissue cultures derived from stem cells that mirror key features of human organs. With the help of Dr. Edward Fon, Scientific Director of the Neuro, Durcan’s team has successfully recreated the most complex organ of all: the brain.

Image by Emilie Hackett.
Brain organoids are minuscule 3D human cell cultures that mirror key features of the human brain. Here, Research Assistant Paula Lépine showcases a brain organoid culture that she personally cultivated.
Serving as the closest available model to patients’ brains, organoids provide a highly precise and innovative approach to studying disease mechanisms and accelerating drug discovery.Brain organoids are an exciting development in neurological research, as they can be personalized using reprogrammed cells from patients. Serving as the closest available model to patients’ brains, organoids provide a highly precise and innovative approach to studying disease mechanisms and accelerating drug discovery.
However, developing these two-millimetre-wide organoids at scale has proven to be challenging.
“The methodology was inconsistent. The organoids varied in size and shape, making it difficult to ensure their health and reproducibility,” explained Durcan. “We wondered if we could standardize the process and scale up production while also reducing the time-consuming and physically taxing workload in the lab. We needed a better system.”
With support from CQDM, HBHL and NeuroSphere, Durcan’s team collaborated with Christopher Moraes, Associate Professor in the Department of Chemical Engineering, to scale up the organoid production process for testing potential therapeutics.
By growing the organoids on biofabricated disks and incubating them in large bioreactors, the team can now control and standardize brain organoid growth, generating over 800 organoids at once. This streamlined approach not only cuts costs and saves time but also facilitates the production of patient-specific organoids, improving the potential for personalized treatments in variable diseases like PD.
“Parkinson’s isn’t determined by one gene. It’s basically an umbrella term—there are over 100 genes to Parkinson’s,” explained Durcan. “Our goal is to explore these different genes with advanced imaging tools and expanding into an automated 3D imaging platform. We started with a biology problem that became an engineering problem and is now becoming a data problem. With countless terabytes of data from 3D imaging these organoids, the next frontier will be applying artificial intelligence towards reconciling all the data and identifying disease signatures.”
The COVID-19 pandemic is partially to blame for this advancement, as limited lab access in March 2020 presented the team with a difficult decision. Nguyen-Vi Mohamed, a postdoctoral fellow at the time, first pitched the idea of combining the biofabricated disk and bioreactor technologies.
Research Assistant Paula Lépine describes this as a significant leap of faith: “Our old method of production involved feeding the organoids at least three times a week. We had to reorganize everything. We transferred all the organoids in large bioreactors that could contain hundreds. Either we took a chance, or we lost them all,” she said.
As a result, the team’s research was unexpectedly accelerated. “We scientists like to take our time and look at all the variables,” admitted Durcan.“But we were forced to test our theory and hope for the best. The culture stayed alive, and we were able to use them in the fall of 2020. We’ve continued with this process ever since.”
The open science approach adopted by Durcan’s team ensures transparency and accessibility for the broader scientific community: their methodology is available online in multiple languages and formats. “Our goal was to build and improve these processes and workflows, applying them into a real translational discovery pipeline. We’re currently building a portal with the data on the cell lines and the modules,” he noted.
As this new technology gains traction, collaborative efforts in knowledge translation are crucial for progress in PD research. “The scientific community is coming to accept that organoids can be used beyond neurodevelopmental studies: they are a useful model for neurodegenerative diseases,” remarked Lépine.
A testament to the potential of brain organoids, Durcan’s team is now working with Western University to identify promising treatments against PD with a new testing platform called TRIDENT. This open science partnership allows the team to leverage and distribute data collected from the organoids.
“We contribute insights that propel the research forward in the knowledge translation pipeline. These synergies allow our partners to conduct additional testing and research of therapies,” said Durcan. This collaborative effort is poised to accelerate the discovery process for PD and foster a dynamic ecosystem for breakthroughs and innovations in the field.
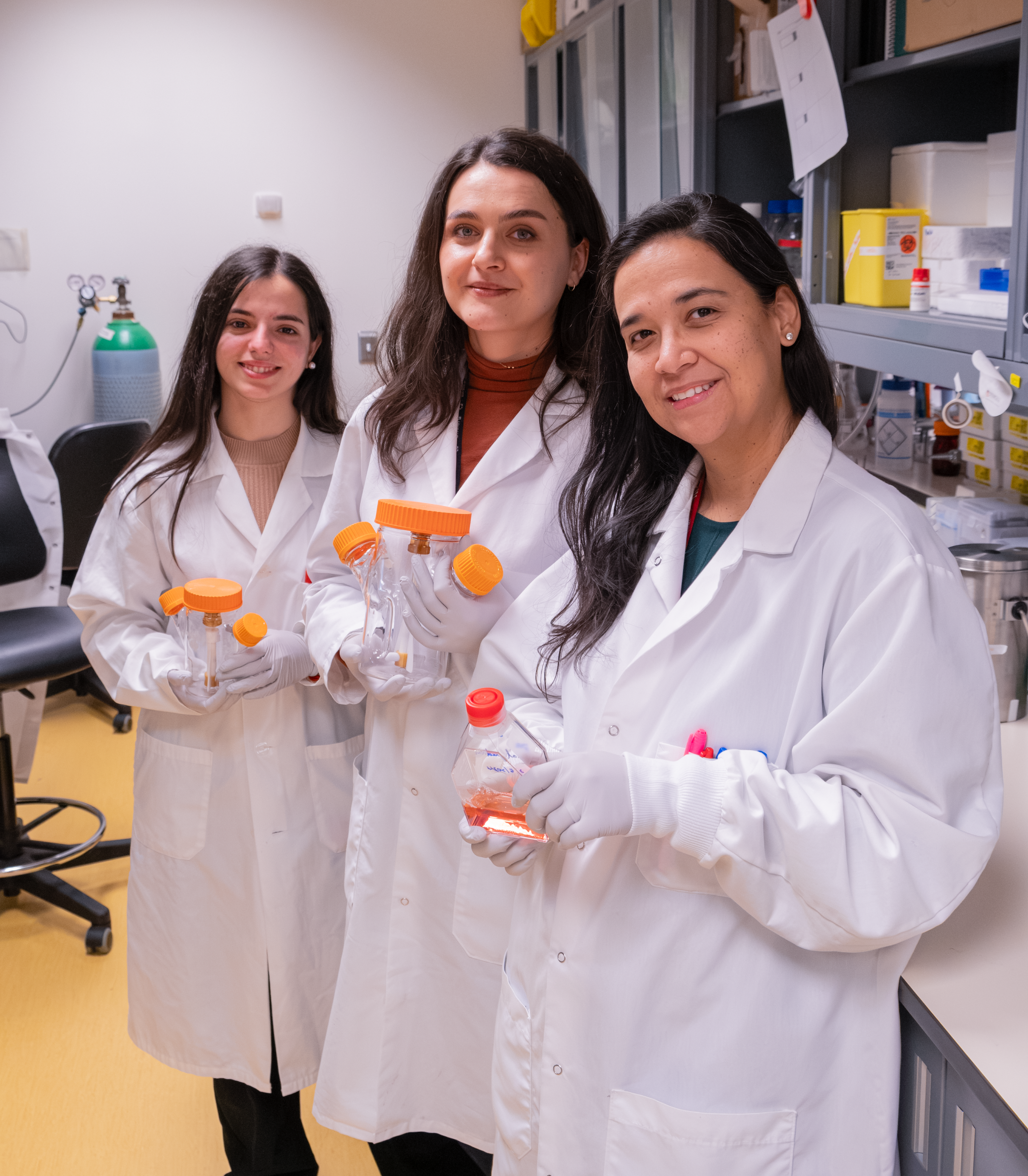
Image by Emilie Hackett.
From left to right: Research Assistants María Belén Baeza Trallero and Paula Lépine and Research Associate Cecilia Rocha. Trallero, Lépine and Rocha are integral members of the team dedicated to advancing brain organoid technology.







