Veronika Pak on Distinctive whole-brain cell types predict tissue damage patterns in thirteen neurodegenerative conditions
My dad and I once took a road trip, all the way from Nova Scotia to Montreal. As we drove past the Montreal Neurological Institute (MNI), we saw a gigantic poster labeled 'THE NEURO,' which was there back in 2017. I told him about all the groundbreaking discoveries that had occurred at the MNI, shaping the very core of neuroscience and neurology. He turned to me and said, "Maybe you'll study there one day?". My dad sacrificed a lot for me to move from Kazakhstan to Canada, all to give me a brighter future. Fast years forward, and there I was at the MNI, a graduate student at the Neuroinformatics for Personalized Medicine (NeuroPM) Lab. After navigating hurdles of immigration and a post-COVID job market while wrestling with social anxiety, I made it.
The first two months of my master’s program at McGill seemed like a blur. Those days were a delightful mix of sunny weather, indulging in pain au chocolat from local bakeries, and exploring the neighborhoods of Plateau and Mile End. However, I could not help but experience imposter syndrome. Other students in my field seemed to have been developing sophisticated deep learning or mathematical models since their third year of undergrad, even if it was not true, while I—let's be honest—couldn’t even fully grasp what my project was about.
I still remember that moment in early November, after reading many relevant papers and preparing my application for the CGS-M, when everything clicked. Everything made sense. From that point on, data analysis for my project felt like smooth sailing. We created whole-brain maps of cell type densities and identified significant associations between the spatial distributions of glial cells in the brain and regional atrophy patterns in 13 neurodegenerative conditions.
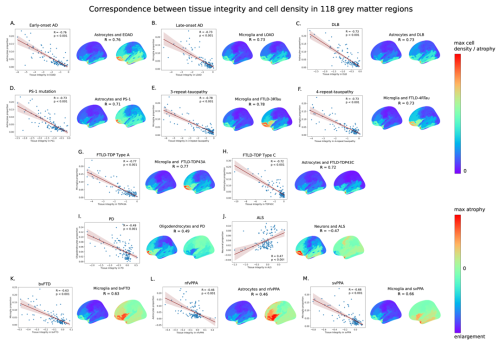
Figure 1. Spatial associations between tissue integrity and cell type proportions for 13 neurodegenerative conditions illustrated in the scatterplots and surface maps (left hemisphere; lateral view) of regional measures.
To create our cell type maps, we used a multimodal approach, merging the fields of neuroimaging and bioinformatics. Previously, senior PhD student Quadri Adewale predicted gene expression across the whole brain using 3072 post-mortem brain samples from the open-access Allen Human Brain Atlas. I applied a cellular deconvolution algorithm to predict cell-type densities from bulk gene expression data and modeled densities to reflect variations in gray matter. Our collaborators, Dr. Yashar Zeighami and Dr. Mahsa Dadar, kindly shared atrophy maps for common neurodegenerative conditions.
To interpret our results correctly, I dove into a rabbit hole of neurodegeneration lore. This journey turned out to be very intriguing since the causes of neurodegenerative diseases remain a big mystery, and no disease-modifying treatments have been fully shown to be effective. Existing therapies can only alleviate symptoms for some patients.
What comes to your mind when you hear about Alzheimer’s disease? Perhaps a cloud of textbook terms like “neuronal loss,” “memory deficits,” “amyloid beta plaques,” “tau tangles,” and “aging as a risk factor”. But what if I told you that the contribution of glial cells is just as important?
When I first encountered glial cells in a systems neuroscience class, the textbook described their role in supporting neurons, and if I remember correctly, they were barely mentioned again. Historically, the relevance of glial cells has been overlooked. Some reviews I read even dared to call them “the janitors of the brain”. Yet, recent breakthroughs in genomics and multi-omics studies, including single-cell analyses of diseased brain tissue, have revealed their significant roles in the progression of neurodegenerative diseases.
The role of glial cells in the brain is highly versatile; just as astrocytes and microglia can support neurons and clear toxic misfolded proteins, they can also release neurotoxic factors that lead to neuronal dysfunction and the accumulation of these proteins.
Our research has echoed this trend in the field of neurodegeneration by showing that brain regions with higher proportions of non-neuronal cells—astrocytes and microglia—might be more susceptible to neurodegenerative processes leading to atrophy. My supervisor Dr. Yasser Iturria-Medina concluded in our manuscript that it’s time for researchers to stop viewing brain diseases through a purely neuro-centric lens. Instead, we should look at the glial and other brain cell types more closely to discover effective, cell-specific therapeutic targets to treat neurodegenerative conditions.
The paper was recently published in eLife. A combination of luck, curiosity, and excellent mentorship helped me publish this paper as a first author during my Master’s, for which I am immensely grateful. The curiosity about the associations between cell types and neurodegenerative diseases and the desire to help patients with dementia inspired me to fast-track to PhD and continue my journey with the NeuroPM Lab.
Speaking of life coming full circle again, I remember how excited I was to attend my first-ever conference, the OHBM international conference, in Montreal back in 2020, and equally bummed when it was moved online due to the pandemic. At the time, I knew nothing about how to navigate the academic world and needed a lot of guidance about how to write a simple abstract or make a poster. Yet, life came full circle when, three years later, the conference returned to Montreal. This time, I had the honor of presenting our findings about cell-type vulnerability to neurodegeneration on stage as a speaker.
The conference helped us attract attention to our cell type maps, which we published on our lab’s Github page. If you work in the neuroimaging field, you can use these maps to see cell-type-specific correlates with your own data. We hope these maps can reveal the contribution of glial cells to other neurological conditions and physiological processes.

OHBM July 2023.