Orçun Haçariz is awarded the 2023 Rodney Collier Junior Research Award
Congratulations to the CRP’s Orçun Haçariz (PostDoc in Dr. Brodt's laboratory) for receiving the 2023 Rodney Collier Junior Research Award for his outstanding contribution to pancreatic cancer research. This award was announced at the recent National Pancreas Conference orchestrated by the Craig’s Cause Pancreatic Cancer Society, a prominent national charity in Canada.
For more on the Craig’s Cause Pancreatic Cancer Society visit: www.craigscause.ca
RI-MUHC trainee honoured by the American Association for Cancer Research
Yasmine Benslimane is investigating how the female hormone estrogen influences the spread of colon cancer to the liver

Yasmine Benslimane, M.Sc. trainee at the Research Institute of the McGill University Health Centre (RI-MUHC), has received the Doren J. Putrah Cancer Research Foundation Scholar-in-Training Award from the American Association for Cancer Research (AACR) to present her work at the AACR Annual Meeting, which took place in New Orleans, LA, in April 2022. Her research project, “Estrogen regulates the Immune Microenvironment of Liver Metastases,” is supervised by Pnina Brodt, PhD, senior scientist in the Cancer Research Program at the RI-MUHC.
“By joining Pnina Brodt's laboratory, I had the perfect opportunity to explore my passion for immuno-oncology and endocrinology,” says Benslimane. “Being able to look at cancer not as a single cellular entity, but rather as part of a complex microenvironment involving multiple actors – such as immune cells and cytokines – made me realize that effective therapeutic strategies can be designed to target these multiple environmental actors. I am grateful to receive this award to present my work at the AACR Annual Meeting.”
“In her project, Yasmine is investigating how the female hormone estrogen is influencing the spread of colon cancer to the liver,” explains Pnina Brodt. “Her work could lead to new treatments for aggressive colon cancer and other cancers that metastasize to the liver and thereby improve patients’ prognosis.”
Adds Benslimane, “Specifically, I am identifying key immune cells and factors that could enhance tumour outgrowth in the liver. My findings that pure anti-estrogen therapy reprogrammed the tumour microenvironment in the liver and could markedly decrease tumour outgrowth thrilled me and encouraged me to present these results to the AACR community.”
The Scholar-in-Training Awards are highly competitive and recognize outstanding young investigators presenting meritorious proffered papers at the AACR Annual Meeting.
RI-MUHC study shows impact of combinatorial immunotherapy on an aggressive cancer
A combinatorial immunotherapy may provide significant therapeutic benefit in managing pancreatic ductal adenocarcinoma liver metastases, preclinical research shows
SOURCE: RI-MUHC. Recently published in Molecular Cancer Therapeutics, work by researchers from the Research Institute of the McGill University Health Centre (RI-MUHC) may open the door for new treatments for an aggressive cancer known as pancreatic ductal adenocarcinoma (PDAC).
PDAC is currently the fourth leading cause of cancer-related deaths in the industrialized world. The prognosis for PDAC patients is currently very poor, with a high incidence of postoperative recurrence, mainly in the liver. Promising advances in cancer immunotherapies such as the PD-1 blocking antibody have not so far proven effective in the treatment of PDAC. This is due, at least in part, to the presence of specific cells that suppress the immune response to this therapy, including myeloid-derived suppressor cells (MDSC). Therapeutic approaches targeting these immunosuppressive cells, particularly in the liver, could enhance the efficacy of immunotherapy and improve prognosis.

Study authors Masakazu Hashimoto, Stephanie Perrino, Andrew M. Lowy and Pnina Brodt
A team led by Pnina Brodt, PhD, senior scientist in the Cancer Research Program at the RI‑MUHC, approached the problem by using a newly bioengineered inhibitor, the IGF-Trap, which blocks type 1 insulin-like growth factor receptor (IGF-IR) signaling. Her team and others had previously shown that immunosuppression within the tumour microenvironment is enhanced by the IGF signaling pathway. The researchers therefore asked whether this novel inhibitor could reverse the suppressive effect of IGF and allow immune cells to act against the tumour, thus enhancing the efficacy of immunotherapy for PDAC.
“We found that by targeting the IGF system, we were able to profoundly alter the immune landscape of PDAC metastases in the liver,” says Dr. Brodt. “As a result, the effect of a PD-1 blocking antibody was enhanced, causing a marked reduction in metastatic tumour growth.”
“Using a murine model, we treated microscopic PDAC liver metastases with the IGF-Trap,” explains first author Masakazu Hashimoto, PhD, a postdoctoral fellow with Pnina Brodt at the time of this study. “We found that this treatment reprogrammed the local immunosuppressive tumour microenvironment in the liver.”
Measuring the impact of the treatment on different types of cells in the immune system, the researchers found that the recruitment of myeloid derived suppressor cells was curtailed. “At the same time, there was an increase in recruitment of killer T cells and in the ability of dendritic cells to activate T lymphocytes,” says Dr. Brodt. “This had the effect of inhibiting metastatic expansion.”
The team then combined the IGF-Trap with an antibody to mimic immunotherapy drugs currently in use in treating cancer patients. They found that the two treatments combined were much more effective than either is alone. In effect, the IGF-Trap potentiated the tumour cell-killing potential of T lymphocytes to help eradicate liver metastases in the murine model.
“These exciting discoveries advance our understanding of how pancreatic cancer cells evade the immune system,” says co-author Andrew Lowy, MD, of the Moores Cancer Center in La Jolla, California. “The IGF-Trap can sensitize pancreatic cancer cells to current immunotherapies, findings that will hopefully be tested in patients.”
“Our results show that a combinatorial immunotherapy could provide a significant therapeutic benefit in the management of PDAC metastases,” concludes Dr. Brodt. “We are thrilled that this effect could be demonstrated with our IGF-Trap. Having established the benefit of this approach in a preclinical model, we hope it will open the way for additional treatments based on this prototype and eventually lead to clinical trials and new treatments for PDAC and other immunotherapy-resistant cancers.”
About the study:
Read the publication in the Molecular Cancer Therapeutics
The authors gratefully acknowledge support from the MUHC Foundation, the Canadian Institutes for Health Research, and MITACS.
November 22, 2021
Pnina Brodt receives Lifetime Achievement Award from the University of Ottawa - December 2020
Alumni Award of Distinction winner conducts research on the biology of cancer metastasis at the RI-MUHC.
Source: RI-MUHC. Pnina Brodt, PhD, was recently honoured with the Alumni Award of Distinction for Lifetime Achievement from the University of Ottawa's Faculty of Medicine, where she completed her M.Sc. The award was presented at a virtual ceremony for the 2020 awards on December 10.

The Faculty of Medicine at the University of Ottawa is where my journey as a scientist began,” she says. “It is in the Department of Microbiology and Immunology that I undertook my first independent research project and published my first scientific paper. I am honoured and immensely grateful to be recognized by my alma mater.”
Pnina Brodt is a professor in the Departments of Surgery, Medicine and Oncology at McGill University and the McGill University Health Centre (MUHC), where she has worked since 1983. Her research has focused on the biology of cancer metastasis, particularly the molecular events that underlie the process of liver metastasis. A senior scientist in the Cancer Research Program at the Research Institute of the MUHC, she previously served as co-leader of its Cancer Axis. She is also a co-founder of the Liver Metastasis Research Network—a multidisciplinary international network dedicated to uncovering the molecular mechanisms of liver metastasis for the betterment of patient care.
She has authored or co-authored numerous publications in such prestigious scientific journals as Nature, Nature Communications, Oncogene, British Journal of Cancer, Clinical Cancer Research, Cancer Research, Journal of Clinical Investigations, Molecular Cancer Therapeutics International Journal of Cancer and Seminars in Cancer Biology. She edited several books on cancer metastasis and holds two patents on a novel IGF receptor inhibitor bioengineered by her team.
Sexual dimorphism: The female hormone estrogen may facilitate the growth of liver metastases in non-sex-specific cancers
January 16th, 2020

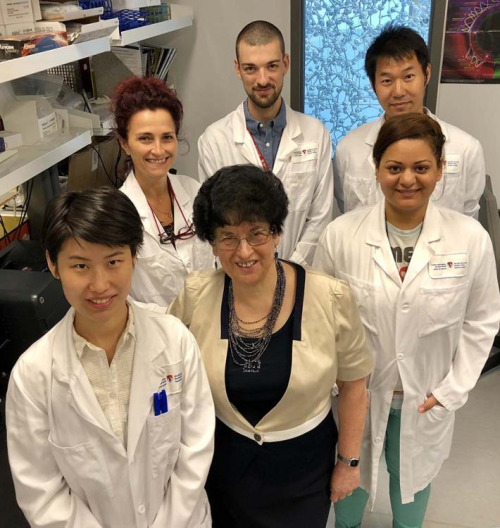
Dr. Pnina Brodt (centre) with some co-authors of the study "Sexual dimorphism and the role of estrogen in the immune microenvironment of liver metastases", from left to right: Ni Wang, Stéphanie Perrino, Simon Milette (first author), Masakazu Hashimoto and Shu Qi.
Montreal - It is known that the tumour microenvironment plays an important role in the progression of cancer. But could estrogen present in this microenvironment facilitate the growth of liver metastases in women affected by colon, pancreatic and lung cancers? This is what a team of researchers from the Research Institute of the McGill University Health Centre (RI-MUHC) suggests, in a study that shows for the first time that the liver immune microenvironment reacts to metastatic cells differently in maleand in female mice and that, indeed, the main female hormone estrogen can indirectly contribute to the growth of metastases. Their findings, recently published in Nature Communications, provide a rationale for further exploration of the role of sex hormones in female cancer patients and the potential benefits of anti-estrogen drugs such as tamoxifen in the treatment of hormone-independent cancers that metastasize to the liver.
“What prompted us to begin this investigation was our finding that the immune microenvironments of liver metastases in male and female mice are regulated differently,” says Dr. Pnina Brodt, senior scientist in the Cancer Research Program at the RI-MUHC and lead author of the study. “We were also aware of reports based on recent immunotherapy clinical trials that female patients do not respond to immunotherapy as well as male patients and that overall, patients with liver metastases respond more poorly to such treatments than patients without liver metastases.”
“We therefore wanted to identify factors unique to male and female responses to liver metastatic disease that could explain these findings and could eventually lead to improved immunotherapy outcomes for patients,” adds Dr. Brodt.
Dr. Brodt and her team looked at the interaction between metastatic cells entering the liver and the unique microenvironment of this organ, in mouse models of colon, pancreatic and lung carcinoma, malignant diseases that do not have a clear sex bias and are not dependent on sex hormones for growth.
By increasing and decreasing the levels of estrogen in their mouse models, the team discovered that estrogen plays a role in the expansion of liver metastases—a major cause of cancer-associated death. Specifically, they found that this hormone regulates the accumulation in the liver of bone marrow-derived innate immune cells such as the myeloid-derived suppressor cells (or MDSC) and immunosuppressive macrophages.
Cancer cell killers can become friends of the enemy
When metastatic cells enter the liver, innate immune cells are recruited, some from the bone marrow. These cells have the ability to kill cancer cells, but once in the tumour environment, they can also acquire immunosuppressive and tumour promoting functions.
MDSCs, for instance, do not directly affect cancer cell growth, but can do so by changing the microenvironment around the tumour in the liver.
“MDSCs can impede the activity of T lymphocytes, whose role is to kill the cancer cells. In this way, they act to promote—rather than curtail—the growth of metastases,” explains Dr. Brodt, who is also Professor in the Departments of Surgery, Oncology and Medicine at McGill University.
The team observed that estrogen induces an immune tolerant environment that helps the tumour cells grow, and that the removal of estrogen reduces the accumulation and activity of MDSCs that, in some way, become “friends” of the enemy.
“The realization that cancer is a community of cells, not just the cancer cells, but also the cells that surround it has become an important part of how the scientific community now views cancer and how it should be treated,” says Dr. Brodt.
Towards gender-specific cancer treatment?
In this era of personalized cancer management and with the worldwide effort to develop drugs that target the tumour microenvironment, awareness of the fact that male and female patients may respond differently to such treatments is very important.
“This should now be taken into account to design better, more gender-specific treatment strategies, especially when we know that colorectal cancer incidence, for instance, is increasing in the younger population,” says Dr. Brodt.
There are several approved anti-estrogen drugs currently in routine clinical use. However, their use is restricted to patients with hormone-sensitive cancers such as breast cancer.
Further investigation is warranted to determine if estrogen plays the same role in cancer patients, and if low toxicity anti-estrogen drugs such as tamoxifen could be used in conjunction with immunotherapy to neutralize the immunosuppressive environment in patients who have non-sex-specific cancers, are premenopausal and have higher levels of estrogen.
About the study
The paper “Sexual dimorphism and the role of estrogen in the immune microenvironment of liver metastases” was written by Simon Milette, Masakazu Hashimoto, Stéphanie Pérrino, Shu Qi, Michely Chen, Boram Ham, Ni Wang, Andrew M. Lowy, Ciriaco Piccirillo and Pnina Brodt. DOI: https://doi.org/10.1038/s41467-019-13571-x
This work was made possible through funding from the Canadian Institute of Health Research, the Québec Ministère de l’Économie, de l’Innovation et des Exportations and the Fonds de recherche du Québec – Santé (FRQS).
Media contact
Fabienne Landry
Communications, Research
McGill University Health Centre
514 812-7722
fabienne.landry [at] muhc.mcgill.ca
Patents by Inventor Pnina Brodt
Pnina Brodt has filed for three patents to protect the following inventions:
Soluble IGF Receptor Fc fusion Proteins and Uses Thereof
U.S. Patent number: 10538575
Abstract: There are described herein novel soluble IGF receptor Fc fusion proteins and compositions and methods of use thereof for treating angiogenesis associated disorders and malignant disease, such as cancer and metastasis, wherein the fusion proteins bind specifically to IGF-1 or IGF-2. Read more...
Type: Grant
Filed: December 14, 2012
Date of Patent: January 21, 2020
Soluble IGF Receptor Fc Fusion Proteins and Uses Thereof
European Patent Registration number: 2791338
Abstract: There are described herein novel soluble IGF receptor Fc fusion proteins and compositions and methods of use thereof for treating angiogenesis associated disorders and malignant disease, such as cancer and metastasis, wherein the fusion proteins bind specifically to IGF-1 or IGF-2. Read more...
Type: Grant
Filed: December 14, 2012
Publication date: February 20, 2019
Therapeutic Applications of Type 1 Insulin-Like (IGF-1) Receptor Antagonists
United States Provisional Patent Application No. 63/120,442.
RI-MUHC researcher receives prestigious provincial grant for innovative project
August 17th, 2018
A researcher from the Research Institute of the McGill University Health Centre (RI-MUHC) has received a Ministry of Economy, Science and Innovation (MESI) grant totaling $250,000 to support the completion of an international collaborative project.
The project is led by Dr. Pnina Brodt, PhD, a researcher who has been studying cancer metastasis for close to 20 years at the RI-MUHC and MUHC and who is a professor in the Department of Surgery, Medicine and Oncology at McGill University. Dr. Brodt’s project is also being supported by the MUHC Foundation.
Ms. Pnina Brodt and her team are hoping to develop a therapeutic strategy to improve the treatment of glioblastoma multiforme—an aggressive form of brain cancer—by optimizing the delivery of a drug she and her lab are developing through the blood-brain barrier.
“We are proud to have committed $250,000 to support Dr. Brodt's research. This investment was instrumental in her ability to secure the prestigious Ministry of Economy, Science and Innovation grant that will allow her to further her groundbreaking research,” says Julie Quenneville, president of the MUHC Foundation. “This is a true demonstration of how philanthropy has the power to drive research and transform care for cancer patients in our community.”
The overarching goal of Dr. Brodt’s project, which she is pursuing collaboratively with biotech firms in Israel (Brainsway), Quebec (Oleotek) and Ontario (Ovensa), is to develop a therapeutic strategy to improve the treatment of glioblastoma multiforme—an
aggressive form of brain cancer by optimizing the delivery of a new drug through the blood brain barrier (BBB).
“Over the years we identified the receptor for the type 1 insulin like growth factor (IGF-1 receptor) as a survival factor for cancer cells, which promotes their growth and increases their resistance to drugs.
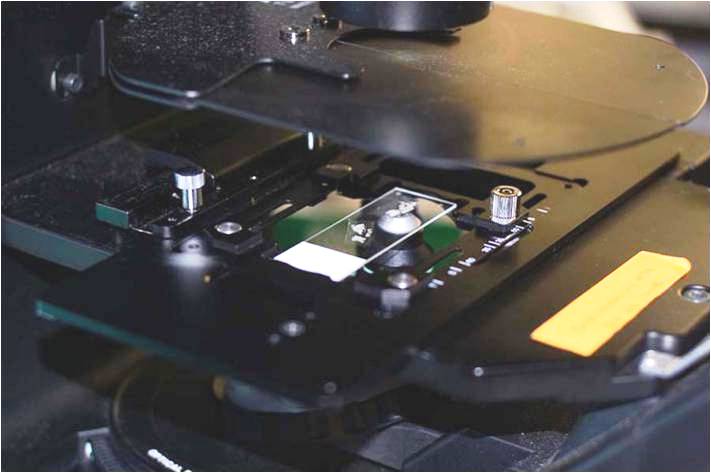
Counting and analyzing cancer cells in Prof. Pnina Brodt’s lab.
This led to the development of the IGF-TRAP that acts as a decoy and in this way reduces the activity of this receptor. We obtained evidence that glioma cells are sensitive to the blockade of the IGF-1 receptor. The problem is that because of its size, the IGF-TRAP cannot easily cross the blood brain barrier and get to glioma cells in the brain. This is a general problem with targeting brain cancers with biological drugs. In this project we will be combining two novel technologies to overcome this barrier to successful treatment of glioblastoma,” says Dr. Brodt.
This is where Brainsway and Ovensa/Oleotek come in. Brainsway developed the Transcranial Magnetic Stimulation (TMS) – an FDA approved technique that can temporarily open the blood brain barrier, while Ovensa and Oleotek are developing nanoparticles (TRIOZAN nanocarriers) that can be used to enable drug delivery through the BBB by adsorption through receptors on endothelial cells. “We will first assess these technologies each separately with the IGF-TRAP and then test them together to see if there is a synergy,” says Dr. Brodt.
If successful, this approach could be used to facilitate the delivery of other drugs to the brain.
Science at its best
Dr. Brodt believes that this type of partnership contributes to the advancement not only of their work, in particular, but to science, in general.
Dr. Brodt’s project was selected in April 2017 as part of MESI’s Research Support Program for international research and innovation initiatives.
Source: McGill University Health Centre (MUHC).
AmorChem invests in a potential therapy for late-stage breast cancer
December 10, 2013
AmorChem gladly announces a new investment in a project focused on the work of Dr. Pnina Brodt, professor in the Departments of Surgery, Medicine and Oncology at McGill University and a researcher of the Cancer Axis at the Research Institute of the McGill University Health Centre (RI-MUHC). The project will be conducted in collaboration with the National Research Council of Canada (NRC) and builds on past collaborative efforts.
January 14, 2014

AmorChem is investing in a project focused on the work of Dr. Pnina Brodt, professor in the Departments of Surgery, Medicine and Oncology at McGill University and a researcher of the Cancer Axis at the Research Institute of the McGill University Health Centre (RI-MUHC).
Dr. Brodt’s work centers on the use of the TRAP technology to inhibit the activity of the type I insulin-like growth factor receptor (IGF-1R), by preventing its binding to its natural ligands, IGF-1 and IGF-2.
The project will be conducted in collaboration with the National Research Council of Canada (NRC) and builds on past collaborative efforts.
Dr. Brodt has been a leader in identifying the important role of the IGF axis in cancer development, invasion and metastasis, and her team’s work in this field is internationally recognized. Her work has led to the development of several strategies for blocking the IGF axis including, most recently, the bio-engineering of a soluble IGF-Trap that is currently being developed as an anti-cancer drug candidate.
Design of the IGF-Trap was refined through collaborative work with NRC, whose protein engineering and production expertise delivered through its biologics program will continue to play an important role in the project.
“Type I insulin-like growth factor receptor (IGF-1R) is recognized today as a validated anti-cancer target, but no satisfactory targeting agent has been developed to date,” says Elizabeth Douville, general partner at AmorChem. “Dr. Brodt’s technology will have clear advantages over existing strategies because it targets the ligands of the IGF-1R without binding insulin. Moreover, Dr. Brodt has generated very compelling data in animal models of lung, colon and breast cancer.”
The IGFs are involved in mammalian growth and development. IGF-1 is essential for many of the growth promoting effects of growth hormone and is involved in the development of normal breast tissue. IGF-1 has been implicated in breast carcinogenesis and was shown to be both anti-apoptotic and pro-mitogenic. It is expected that a decoy receptor (the IGF-Trap) would greatly impact the levels of bio available IGF-1 and IGF-2 at tumour sites, thereby blocking the ir proliferative/anti-apoptotic effects on the cancer cells. [Source: Amorchem.com].