Translational research from fundamental to applied allows to well conceived solutions to be proposed. In regards to spine biomechanics, this system may be assisted or improved via external of internal fixation. That is external corset, braces or exoskeleton may enhance or regulate spine stability or performance. Moreover, the same may come from internal devices.
Past projects
Building upon this fundamental research, the awarded in silico model (awarded 2015 ANSYS Hall of Fame) was now ready for applied research. A spine model was developed to new versions enabling more focused analyses. Many difference spine medical devices were explored via in silico modalities in order to optimize the performance or foster the creation of novel devices patents to address the identified shortcomings. These conceived devices shared in their purpose to manipulate how loads were allocated and distributed within the spine. Hence, these novel devices, conceived as a result of in silico modeling of the spine, sought to alter the biomechanics of the spine.
Current projects
Augmented Reality/ Virtual Reality
The conventional surgical technique of “see one, do one,” has various ethical, cost, and time concerns, as it entails training on live patients. The conventional surgical training systems, i.e. on-patient or cadavers, come with ethical and cost issues that limit the residents in their ability to improve their skills in complicated techniques. Therefore, teaching hospitals are moving towards inanimate training systems using synthetic materials and virtual reality (VR), where the latter is preferred for its ability to provide repetitive and intensive training without requiring replacements.
VR training systems are the conventional training systems in the aerospace industry for pilot training. The success of VR training systems in pilot training has demonstrated its potential in the medical industry towards limiting the complications associated with on-patient training. The technological developments in medical imaging have made the representation of biological tissues in virtual environments possible. VR training systems provide a wide array of options as the users can practice basic surgical techniques to improve their psychomotor skills or practice complete procedures in preparation for an on-patient procedure.
Augmented reality (AR) is the art of combining VR with real world elements, which has been made possible by technological developments that allow 3D representation of the virtual environment to be displayed in the real world. Such technology can provide a lot of information to a surgeon, especially in minimally invasive surgeries, where they have limited access to the operating area and depend on 2D images from a camera to analyze the environment before initiating a surgery.
The main concern most teaching hospitals and doctors have with the use of VR training systems is the ability to transfer skills acquired on these training systems to an operating room (OR) setting. This can be achieved with realistic representation of the mechanics of tissues and organs involved, which are delivered through the visual, haptic, and auditory experience. Haptics provide the user with force feedback, which is especially important in a minimally invasive procedure where doctors have limited access to the operating area. Mimicking those same force feedbacks in a training system would allow the resident to learn not only the technique but also the role of the sense of touch in the procedure.
The versatility of VR training systems and their applications in the medical industry are not limited to surgical training. These systems show potential in surgical planning, telesurgeries, and computer guided surgeries.
Presently, there is a lack of understanding about the mechanical behavior of the tissues of the spine during a surgery. Using this knowledge, realistic mechanical characterization of the surgery can be developed for an interactive VR/AR system. Understanding the mechanics of the biological tissue and their response to manipulation by surgical tools will be used towards the development of a finite element model of the operating area in the virtual environment.
These models will be integrated into a novel, interactive virtual reality training system, which allow surgical residents to practice intensively and repetitively without risking lives of patients. Using parallel processing a realistic interaction and manipulation of the operating area will be developed. This VR/AR training system will utilize physics driven haptics to provide an immersive experience to the users.

In order to create an immersive and believable virtual environment, the link between physical and geometric model will be established. This research plans to apply an algorithm to achieve this link. The algorithm needs the physical model topology, geometric modelling and virtual reality rendering. The physical model uses accurate responses to image data. The geometric model will follow the mesh flow and edge loop, which increases the frame rate and limit the polygon number. The last step for virtual reality rendering requires the final images for end users.
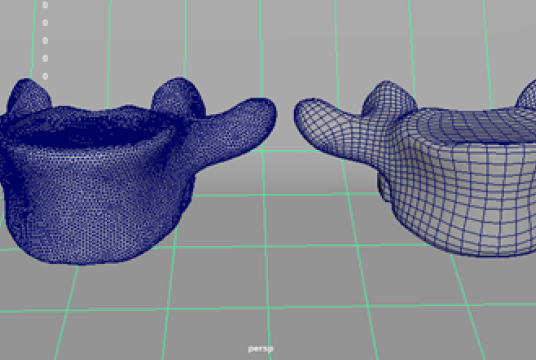
The figure above shows topology processing of a vertebral body (L5). On the left, is a physical model with high accuracy whereas on the right, the geometric model shows low-resolution polygon faces, which is more suitable for a VR or AR environment.