 The McGill Department of Medicine celebrated its 100th anniversary in 2024, marking a century of leadership in medical research, innovative patient care, and transformative education. Since its founding with Dr. Jonathan C. Meakins’ appointment as the first full-time Chair in 1924, the department has evolved into a world-renowned institution.
The McGill Department of Medicine celebrated its 100th anniversary in 2024, marking a century of leadership in medical research, innovative patient care, and transformative education. Since its founding with Dr. Jonathan C. Meakins’ appointment as the first full-time Chair in 1924, the department has evolved into a world-renowned institution.
To mark this milestone, we hosted a series of centennial events - including an awards ceremony, historical features in our newsletter, a history quiz, and a recreation of the iconic “chairs of the department” photo. We’re also giving our Glen site front offices a historical makeover and dedicating our 2024 annual report to the DOM @ 100. Most importantly, we joined forces with current and former faculty to uncover and showcase key moments from our history - discover some of these milestones below.
Methods
While McGill DOM members have contributed to many discoveries and innovations we highlight those that have stood the test of time as important discoveries that have changed clinical practice globally, importantly shaped local care delivery or changed how we train generations of physicians.
Historical Milestones
1819
![]()

Montreal General Opens
The Montreal General Hospital (MGH) had opened in 1819 with funds raised by Montreal’s English community after a failed petition to the Lower Canada House of Assembly to build a second hospital to serve the city’s sick poor. The MMI’s four founders – Dr William Robertson, Dr. John Stephenson, Dr. William Caldwell, and Dr. Andrew Fernando Holmes – all took professorships at the faculty and played important roles in the development of the medical school as well as the improvement of public health in Montreal.
1829
![]()

Birth of a Faculty
The new McGill College received its royal charter from King George IV in 1821. However, the College was soon in danger of losing its charter because, though it had appointed a principal and a few figurehead professors, it hadn’t actually managed to form a faculty in any subject. Meanwhile, the Montreal Medical Institution (MMI), a proprietary medical school established in 1823 by four Montreal General Hospital (MGH) physicians, could issue medical licences to its graduates but couldn’t grant medical degrees because it had not obtained a royal charter. In a mutually beneficial arrangement, McGill College and the MMI merged in 1829. The MMI became the College’s first faculty, and the MGH, from which the MMI had sprung, McGill’s inaugural teaching hospital. Four years after it opened, in 1833, McGill College awarded its first degree – in medicine – to William Leslie Logie. It was the first medical degree awarded in the Canadian colonies.
1893
![]()

Royal Victoria Opens
The imposing Royal Victoria Hospital, built on the southern slope of Mount Royal on land donated in 1887 by rail barons Lords Strathcona and Mount Stephen, opened its doors in 1893. From its founding, the RVH was formally affiliated with McGill University’s Faculty of Medicine, serving as a principal site for clinical training, research, and patient care.
1919
![]()

Osler Advocates for Chair
Sir William Osler, Regius Professor of Medicine at Oxford University, McGill University's most distinguished medical graduate, and the world's most renowned physician, shortly before his death in 1919, recommended that McGill appoint a full-time Chair of the Department of Medicine who would establish research in the hospital as an essential part of academic medical activities. Until then, teachers at McGill's medical school were part-time physicians with private practices outside the teaching hospitals.
1924
![]()

Department Formed
Dr. Jonathan C. Meakins was appointed McGill’s first full-time Professor and Chair of Medicine in 1924, supported by a Rockefeller Foundation grant. Meakins established the department’s research infrastructure at the Royal Victoria Hospital (RVH), creating a model that integrated clinical practice with scientific inquiry. His publication, Respiratory Function in Disease (1925), was among the earliest significant works in pulmonary medicine and set a precedent for research-driven medical education. Meakins’ recruitment of Dr. Ronald Christie in the early 1930s further bolstered McGill’s focus on respiratory physiology, leading to critical publications on lung mechanics and blood gas abnormalities in diseases like emphysema and pulmonary edema.
1924
![]()

St. Mary’s Opens
Irish immigrants poured into Montreal from the mid-19th century, fleeing the devastating famine, and continued to arrive into the early 20th century. Mostly Catholics, these newcomers often had to choose between receiving medical care in English from Protestant institutions, like the Montreal General Hospital, or in French from Catholic institutions, like Hôtel-Dieu. A temporary hospital, St. Patrick’s, was set up to treat passengers from the disease-ridden “fever ships” that brought them from Ireland in the 1850s, but closed after 10 years; two specially-created Irish wards at Hôtel-Dieu did their best to treat Irish Catholics in English until St. Mary’s Hospital (SMH) was founded in 1924. Although McGill medical students and residents had been training at St. Mary’s Hospital Center, as it is now known, for decades, the hospital only became officially affiliated with the university in 2013.
1924
![]()

Women Physicians Unite
Did you know that in Canada, the fight for equity in medicine began in earnest a century ago? In 1924, with the founding of the Federation of Medical Women of Canada (five years before women were legally recognized as persons under Canadian law), Dr. Maude Abbott, the Federation’s founding president, rallied her colleagues to press for change. At that time, medical schools were still reluctant to accept women. Of the approximately 8,000 doctors in Canada, only 187 (2 percent) were women, with many trained abroad in the U.S. or Europe. We have come a long way but don’t yet have gender equity at the top of the professorial ranks and leadership positions.
1934
![]()

Jewish General Opens
The Jewish General Hospital (JGH) opened in 1934 with money raised by the Jewish community. Large numbers of Jewish immigrants arrived in Montreal in the late 19th and early 20th centuries, fleeing religious persecution, mostly in Europe. However, in Montreal they continued to face discrimination accessing care and, in the case of health professionals, getting hired in hospitals. McGill medical students began doing clerkships at the JGH in 1939 and the hospital’s full affiliation with McGill was granted in 1969.
1936
![]()

Congenital Heart Breakthrough
Dr. Maude Abbott’s contributions were pivotal in establishing McGill’s reputation in cardiology. Her Atlas of Congenital Heart Disease (1936), based on extensive research and autopsy specimens from the Montreal General Hospital (MGH), became a foundational text in understanding heart malformations. Abbott’s innovative classification methods greatly influenced clinical approaches to pediatric cardiology and positioned McGill as a leader in the field.
1946
![]()

Peritoneal Dialysis Performed in Canada
In 1946, physicians at the Montreal Jewish General Hospital performed one of the first dialysis treatments in Canada using a primitive artificial kidney. Drs. Morton Korenberg and Joseph C. Portnuff successfully treated a patient suffering from acute kidney failure by employing peritoneal dialysis - a process where waste products are removed from the blood through the peritoneal membrane. This pioneering effort not only saved the patient’s life but also marked a significant milestone in the history of kidney care in Canada, paving the way for modern dialysis techniques.
1948
![]()

First Quebec Hemodialysis
On February 23, 1948, Dr. John MacLean, a Canadian Forces urologist who had started working at the RVH in 1945, performed Montreal’s first hemodialysis using Dr. Kolff’s artificial kidney. That procedure marked the start of a hemodialysis program in Quebec and established the department as a leader in nephrology.
1952
![]()

University Medical Clinic
Using funds raised by the Montreal General Hospital’s new research committee, Physician-in-Chief E.S. Mills opened the University Medical Clinic (UMC) in 1952. The UMC was to have an enormous impact on the hospital’s reputation for research and on the coordination of its activities. Following pressure from McGill to apply the same academic principles of advancement through research as in the Department of Medicine, the MGH recruited H. Rocke Robertson to be Surgeon-in-Chief in 1958. He established the University Surgical Clinic (USC) the following year.
1956
![]()

Advances in Respirology
Dr. Ronald Christie, who returned to McGill as the Chair of Medicine in 1956, played a crucial role in advancing pulmonary research. His tenure saw significant developments, including the co-founding of the Meakins-Christie Laboratories in 1972, which became a hub for groundbreaking respiratory research. These laboratories attracted experts like Dr. David Bates and Dr. Joseph Milic-Emili, whose work on the mechanics of breathing and small airway diseases contributed to global advancements in respiratory medicine.
1957
![]()

Medical Education Innovation
These new research initiatives in the hospital marked the beginning of postgraduate training for a growing population of clinicians. When Mills resigned in 1957, Douglas Cameron became Physician-in-Chief, and set about restructuring the clinical units within the hospital so that they could be close to the hub of research activity at the UMC. Realizing that research and teaching could be more effectively concentrated on a specialty-by-specialty basis, he created Divisions under the Department of Medicine, with geographic-full-time chiefs who acted as McGill professors and directors of research in their various specialties. Subsequently, each Division developed its own lines of investigation, and advanced according to its own trajectory – these are the specializations in medicine and surgery that we recognize today. The activity generated in the medical clinics boosted the academic reputation of the hospital: between 1955 and 1960, the postgraduate training population of the hospital went from fifteen to 250. The hospital continued to attract increasing numbers of researchers from all over the world.
1958
![]()

First Kidney Transplant
Dr. John B. Dossetor pioneered Canada’s first successful kidney transplant between identical twins at the Royal Victoria Hospital. It was the first such life-saving procedure in Canada or in the entire Commonwealth and allowed its recipient to avoid certain death. Although kidney transplantation between identical twins had been performed in 1958, a regular cadaver kidney transplant program began only in 1964. Dr. John B. Dossetor went on to establish the first transplant program at McGill University - one of the earliest in Canada.
1960
![]()

Asthma Treatment Advances
During Dr. Samuel Freedman's tenure at the Montreal General Hospital (MGH), significant advances were made in treating asthma and allergic rhinitis. Initially, treatments included intravenous ACTH and aminophylline, requiring close monitoring due to the lack of blood level measurement methods. The introduction of prednisone in the mid-1960s reduced the need for desensitization treatments. Diagnostic methods evolved, with intradermal and scratch testing being debated before Dr. Jack Pepys' prick test became standard. Additionally, under Dr. Joseph Shuster's supervision, the Clinical Immunology Laboratory introduced advanced testing for autoimmune diseases.
1963
![]()

Liver Metabolic Pathways
Carl Arthur Goresky was an internationally renowned scientist, clinician and teacher whose hallmark 1963 paper, using pure mathematical precision, uncovered many aspects of capillary-tissue exchange in the liver. This discovery brought a new understanding to the liver’s transport network, which allows the organ to metabolize and move materials such as glucose, proteins, and vitamins to tissues in the body that need them. Goresky’s understanding of the liver led to studies of other transport systems in the body’s microvasculature, making him a pioneer in the study of transmembrane transport and intracellular metabolism.
1964
![]()

Code 99 Introduced
In 1964, Dr. Stewart Reid and Dr. John H. Burgess established a roving cardiac arrest team at the Montreal General Hospital (MGH). The first "code 99" attempt faced technical difficulties, but subsequent efforts improved, leading to the development of continuous monitoring for heart attack patients and the creation of the Coronary Care Unit. The first successful resuscitation made headlines in the Montreal Gazette.
1964
![]()

Endocrine Research Advances
In 1964, Dr. John Beck was appointed Physician-in-Chief at the Royal Victoria Hospital and Chairman of the Department of Medicine at McGill University in 1969. He did pioneering work in basic and clinical endocrine research on the pituitary and adrenal glands, hormonal changes in pregnancy, the gastrointestinal hormones influencing pancreatic endocrine function and the hormonal control of adipose tissue metabolism. Much of his energy, while Chair of Medicine focused on undergraduate medical education, residency and fellowship training and advanced training for physicians, primarily destined for academic and leadership roles.
1965
![]()

Colon Cancer (CEA) Marker
In 1965, Dr. Phil Gold and Dr. Samuel Freedman published a paper describing the Carcinoembryonic Antigen (CEA) in tissue from large bowel tumors. This discovery led to the development of a blood test for colon cancer management still used today and gained international recognition.
1966
![]()

Lung Ventilation Perfusion
Dr. Peter Macklem and Dr. Joseph Milic-Emili utilized radioactive xenon-133 to assess regional ventilation and perfusion in the lungs at the Royal Victoria Hospital (RVH) in Montreal. This technique allowed for a better understanding of how different regions of the lung functioned under various physiological and pathological conditions. Their research led to several influential publications, including studies on the regional distribution of gas in the lung, which became one of the most cited papers in clinical research during the late 1960s and 1970s. The success and impact of their research laid the groundwork for the establishment of the Meakins-Christie Laboratories in 1972, with Dr. Macklem serving as the founding director.
1970
![]()

ERCP Introduced Nationally
Dr. Mansour Jabbari was the first to introduce endoscopic retrograde cholangiopancreatography (ERCP) into the country and became a pioneer in the diagnosis and management of diseases of the biliary tree and pancreas.
1970
![]()

Human Prolactin Discovered
While working from 1965 to 1973 in the Polypeptide Lab of the Endocrine Division of the Department of Medicine, Dr. Henry Friesen discovered human prolactin, a hormone which stimulates lactation in mammary glands. Dr. Friesen was a recipient of the 1977 Canada Gairdner International Award. In recognition of his contributions to the understanding of the biochemistry, physiology and pathophysiology of lactogenic hormones and for the identification of human prolactin. His research on growth hormones in childhood dwarfism helped in developing a therapy for this condition and his work with prolactin helped to develop the drug bromocriptine, used for the treatment of infertility.
1970
![]()

Chest Imaging Advances
In 1970, Dr. Bob Fraser and Dr. Peter Paré co-authored “Diagnosis of Diseases of the Chest”, a landmark publication that documented and promoted newly recognized radiological patterns. The book played a pivotal role in shifting diagnostic approaches in pulmonology, from debates over physical signs to a more systematic reliance on pattern recognition. Widely influential, the text not only transformed clinical practice but also reinforced McGill’s reputation as a leader in respiratory medicine.
1972
![]()

Meakins-Christie Established
Established in 1972, the Meakins-Christie Laboratories grew out of Dr. Peter Macklem’s pioneering research that reshaped the understanding of lung function. With strong support from Dr. Ronald Christie, Chair of Medicine from 1956 to 1965, the lab became a leading centre for respiratory research at McGill, with Dr. Macklem serving as its founding director.
1972
![]()

CPR Program Success
The first documented report of improved outcomes from a hospital-wide CPR program led by a trained cardiac resuscitation team from the RVH Division of Cardiology was published in the New England Journal of Medicine in 1972 by Dr. Jean Lemire and Dr. Arnold Johnson.
1973
![]()

Northern Cardiac Outreach
Dr. John H. Burgess initiated monthly cardiac consulting visits and served as the cardiac consultant for the Baffin Region (later Nunavut) and northern Quebec (later Nunavik). He was awarded the Order of Canada in 1987.
1973
![]()

GI Diagnosis Breakthrough
At the Gastrointestinal Research Laboratory at the Royal Victoria Hospital, Dr. Jacques Kessler pioneered the clinical use of breath testing to diagnose upper GI disorders. He also implemented the use of liquid chromatography to detect deconjugated bile salts in endoscopic samples, improving diagnosis of blind loop syndrome in post-gastrectomy patients from earlier decades.
1980
![]()

Hormone Assays Developed
During the 1980s and 1990s, Dr. Beverley Murphy spearheaded research in the Division of Endocrinology and Metabolism. Her early work focused on developing new hormone assays, leading to a breakthrough method for estimating plasma cortisol, which she later applied to thyroxine measurement. Dr. Murphy was the first to identify cortisol deficiency in premature babies with respiratory distress syndrome, leading to a promising treatment. Her cortisol assay method also revealed excess cortisol in depressed patients, prompting successful initial trials of antiglucocorticoid drugs for major depression. Her pioneering assays of cortisol and thyroxine earned her wide recognition and citations.
1984
![]()

Stroke Rehabilitation Research
Dr. Sharon Wood Dauphinee, in collaboration with Dr. Ed Bass and Dr. Harold Frank, conducted early clinical research at the Montreal General and Jewish General Hospitals examining the impact of interdisciplinary team care following acute cerebrovascular stroke. Interdisciplinary team care is a collaborative approach to healthcare in which professionals from different disciplines work together to plan, coordinate, and deliver comprehensive care to patients. This work laid foundational evidence for the benefits of coordinated, multidisciplinary stroke rehabilitation.
1985
![]()

Diabetes Pathway Discovered
Dr. Barry Posner’s work in endocrinology, particularly his discovery of the endosomal system in insulin signaling, revolutionized understanding of cellular receptor functions. He discovered that a part of the cell called the endosomal system plays a key role in how cells respond to insulin. He also found how certain enzymes help control this process. His work helped pave the way for better treatments for diabetes and other metabolic diseases. Later, he served as Physician-in-Chief at the Jewish General Hospital from 1996 to 2002.
1985
![]()
First Immunodeficiency Clinic
In late 1985, as the AIDS epidemic spread globally at increasingly alarming rates, the MGH opened a clinic dedicated exclusively to the care of AIDS patients, directed by Dr. Christos Tsoukas. The AIDS Clinic – later renamed the Immune Deficiency Treatment Centre – was the first of its kind in Canada, bringing together immunologists, psychiatrists, infectious disease specialists, dermatologists, and other professionals. In addition to multidisciplinary treatment, the clinic provided counselling to patients and their families, performed diagnostic testing, and collaborated on awareness-raising campaigns. Dr. Tsoukas identified the first case of transfusion-related AIDS transmission in Canada and, through his studies on hemophiliacs, was instrumental in the establishment of blood safety protocols outlined in the Krever report.
1986
![]()
Pulmonary Hypertension Clinic
Dr. David Langleben established the first Pulmonary Hypertension clinic in Canada. Dr. Langleben has been involved in several global clinical trials and was part of teams that brought innovative therapies to patients with pulmonary hypertension. His contributions to research on nitric oxide, endothelin receptor antagonists, and phosphodiesterase inhibitors have shaped the standard of care for PAH patients worldwide.
1990
![]()

HIV Treatment Transformed
At the Jewish General Hospital (JGH), Dr. Mark Wainberg is best known for his discovery of lamivudine (3TC), a key antiretroviral drug used in the treatment of HIV/AIDS. His work revolutionized HIV treatment by making it more effective and accessible. Lamivudine became a cornerstone of antiretroviral therapy, significantly improving the lives of millions of people living with HIV around the world. In addition to this discovery, Dr. Wainberg made significant contributions to HIV research, including studying drug resistance and advocating for global access to HIV treatment. He was also a strong advocate for human rights and the fight against HIV/AIDS stigma.
1994
![]()

BRCA1 Gene Isolated
In 1994, Dr. Steven Narod and his postdoctoral fellow, Dr. Patricia Tonin, contributed to a landmark international study that successfully identified the BRCA1 gene, responsible for hereditary breast and ovarian cancer. Their findings were published in Science and garnered widespread media coverage, including a McGill News feature titled "Race of Life." This discovery marked the culmination of a global search for the gene that had begun in 1990.
1997
![]()

MUHC Officially Formed
Pressure on the network to consolidate administration and medical services resulted in the voluntary merger in 1997 to form the McGill University Health Centre (MUHC). The MUHC brought together the Montreal General Hospital and the Royal Victoria Hospital – the two finally putting aside their old rivalries – as well as the Montreal Neurological Institute-Hospital, the Montreal Chest Institute and the Montreal Children’s Hospital. The Lachine Hospital came on board in 2008. The MUHC made a historic move to its new location, the Glen site, in 2015, with the Royal Vic, the Children’s and the Chest Institute housed under one roof.
2001
![]()

Hypertension Research Leader
Dr. Ernesto Schiffrin, former Associate Chair and a distinguished James McGill Professor, has made significant contributions to hypertension research. His work on the renin-angiotensin-aldosterone system led to advancements in the development and use of ACE inhibitors and angiotensin II receptor blockers. Schiffrin’s research has influenced global hypertension treatment protocols, which are now mainstays of hypertension management.
2004
![]()

Bone Metabolism Breakthrough
From 1994 to 2004, Dr. David Goltzman, was Chair of the Department of Medicine. He was also Physician-in-Chief at the Royal Victoria Hospital from 1994 to 1998 and of the McGill University Health Centre from 1998 to 2004. His research has mostly focused on the hormonal regulation of mineral and skeletal homeostasis, including the function of parathyroid hormone, especially its function as an anabolic agent; parathyroid hormone-related protein, where he elucidated the sequence of the human gene and the role of this protein in anabolic actions on bone; and on the mechanism of action of vitamin D. He has also made major contributions to our understanding of metabolic bone diseases including osteoporosis, and he has led the Canadian Multicentre osteoporosis Study(CaMos).
2007
![]()

Breast Cancer Gene Identified
In 2007, Dr. William Foulkes and his team at McGill helped identify PALB2 as a breast cancer susceptibility gene, contributing to the understanding of its role in hereditary breast cancer. While PALB2 mutations are rare, they can be significant in certain populations, such as Finland, where a founder mutation is present. A leading figure in cancer genetics at McGill for over 30 years, Dr. Foulkes is a Fellow of the Royal Society of Canada and one of the most highly cited researchers in the Department of Medicine. He currently serves as Chair of the Department of Human Genetics and is a recipient of the Wilder‑Penfield Prix du Québec for his contributions to medical research.
2018
![]()

Rifampin Guidelines Updated
Two landmark companion articles led by Dr. Dick Menzies and published in the New England Journal of Medicine demonstrated that rifampin is a safe and effective treatment for latent tuberculosis infection in both adults and children. The trials showed that rifampin had a better safety profile than isoniazid, the previous standard treatment. These findings led to rifampin being recommended as the first-line treatment of latent tuberculosis by the Canadian Thoracic Society, the Public Health Agency of Canada, the American Thoracic Society, the Infectious Diseases Society of America, and the World Health Organization.
2020
![]()

Campus Outaouais Opens
McGill continued to build on the work it had begun in Outaouais in 1988, to address the chronic doctor shortage in the region. In 2010, a new program welcomed McGill medical students in the third year of their studies. Five years later, a clinical plan was developed that would see the entire McGill medical program offered to students in the region. In August 2020, the new Campus Outaouais welcomed its first cohort – 24 first-year McGill medical students and, in collaboration with the Faculty of Science and the Université du Quebec en Outaouais, 16 students in a specially designed pre-med preparatory program. By 2024, there will be 96 McGill students enrolled in the first four years of the medical program, some 20 students in the preparatory program, and 50 residents and interns. In all, close to 170 McGill students will be living in the region.
2024
![]()

Collaborative Research Strengthened
McGill’s modern approach to interdisciplinary research was highlighted by the establishment of the “World-Class Teams” initiative, fostering collaboration among experts in various medical fields. This initiative exemplifies the department’s ongoing dedication to translating research into clinical practice to address emerging health challenges.
2024
![]()

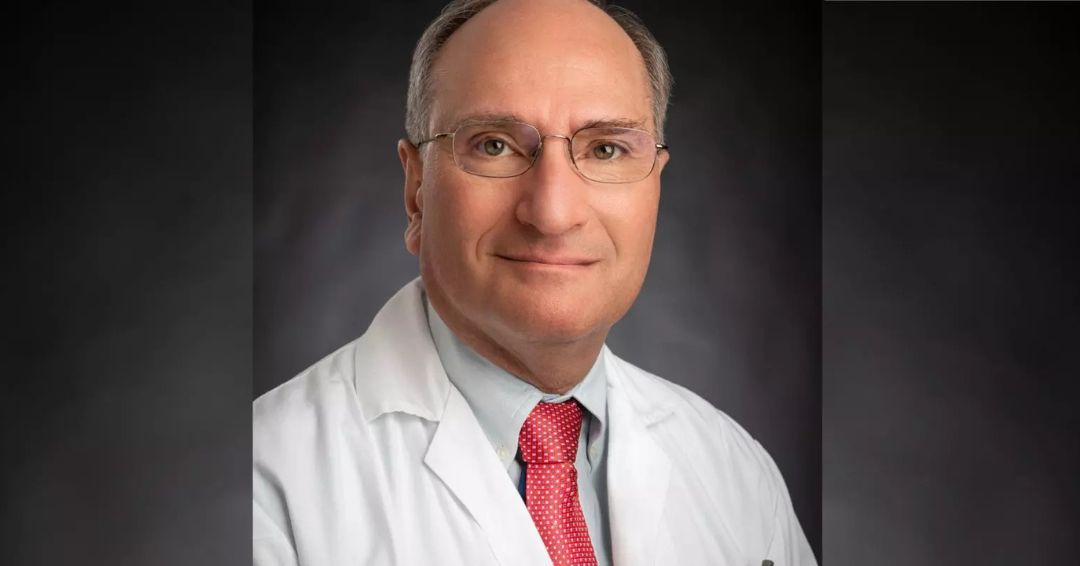
Graduate Program Expansion
In line with the McGill Department of Medicine’s 2024-2029 Strategic Plan, and under the leadership of Chair Dr. Marc Rodger, the Graduate Program in Experimental Medicine has been expanded and renamed the Graduate Program in Clinical and Translational Research. The purpose of this rebranding is to ensure the program title reflects the contemporary breadth of research within the Department and supports the vision of becoming the “Most Research Intensive DOM in Canada.” The new Graduate Program in Clinical and Translational Research will be divided into three streams: 1) Experimental Medicine, 2) Digital Health Innovation, and 3) Clinical Research.
Leadership Timeline
We can trace back the origins of the Department of Medicine to “1845, when the chair of clinical medicine was established.”1 The number of staff in the Department has increased gradually over the years, from one faculty member in its early years to 800 today. In 1924 Jonathan C. Meakins was the first to obtain the title of Chair of the Department.2 His successor, J. S. L. Browne, took over in 1948. In the 1950s and 1960s, Experimental Medicine and Investigative Medicine existed as separate departments, the first created by Jonathan C. Meakins and the other by Ronald V. Christie.3 In the 1969-1970 academic year, the Department of Investigative Medicine was merged with the Department of Experimental Medicine. Experimental Medicine was integrated into the Department of Medicine at the end of the 1970s.
McGill Department Heads |
RVH Physicians-in-Chief |
MGH Physicians-in-Chief |
MUHC Physicians-in-Chief |
|
1924-1947 |
1924-1942 Jonathan C. Meakins
|
1950-1957 |
1998-2004 |
|
1948-1955 |
1947-1952 G. Raymond Brow |
1957-1980 |
2004-2011 |
| 1956-1965 Ronald V. Christie |
1952-1955 Walter de M. Scriver |
1980-1995 1995-1998 |
2012 - 2013 |
| 1965-1969 Douglas G. Cameron |
1955-1964 |
2014 - 2019 |
|
| 1969-1975 John C. Beck |
1964-1974 John C. Beck |
2020 - Present Marc Rodger |
|
| 1975-1980 Douglas G. Cameron |
1974-1979 Maurice McGregor |
||
| 1980-1985 Peter T. Macklem |
1979-1986 Peter T. Macklem |
||
| 1985-1990 Phil Gold |
1987-1993 W. Dale Dauphinee |
||
| 1990-1993 W. Dale Dauphinee |
1994-1998 David Goltzman |
||
| 1994-2004 David Goltzman |
|||
| 2004-2011 David Eidelman |
|||
| 2012 - 2013 James Martin (interim) |
|||
| 2014 - 2019 James Martin |
|||
| 2020 - Present Marc Rodger |


1McGill University for the Advancement of Learning, Volume II 1895-1971, Stanley Brice Frost, McGill-Queen’s University Press, 1984, p. 385.
2McGill University Calendar, 1924-1925, p. 330.
3McGill University for the Advancement of Learning, Volume II 1895-1971, Stanley Brice Frost, McGill-Queen’s University Press, 1984, p. 385-386.
Faculty Growth
Faculty members
1860-1861
Member: 1
1900-1901
Members: 4
1945-1946
Members: 51
1975-1976
Members: 241
1985-1986
Members: 424
1995-1996
Members: 695
2005-2006
Members: 700
2009-2010
Members: 800
2011-2020
Members: 811
2021-2023
Members: 839